Universal Health Coverage
Objective
On the strong platform of Pradhan Mantri - Jan Arogya Yojana (PM-JAY):
Attain a coverage of at least 75 per cent of the population with publicly financed health insurance (covering most secondary and tertiary care procedures) by 2022-23.
Reduce by 50 per cent the proportion of households facing catastrophic health expenditure from the current levels.
Current Situation
There have been noteworthy strides over the past two decades in the quality of health care delivered to citizens and population health outcomes. Yet, there is wide variation across states in the availability of resources, the status of state health programmes, rural-urban differentials and governance capacity.
Public health infrastructure in the country expanded considerably following the launch of the National Health Mission in 2005; however, there continues to be a shortfall in several areas. In 2015, the number of sub-centres (SCs) fell short of requirements by 20 per cent, of primary health centres (PHCs) by 22 per cent and of community health centres (CHCs) by 32 per cent in rural India. The quality of public sector health facilities has also suffered because of shortage of personnel and lack of necessary supplies.
Data from the National Sample Survey Organisation’s 71st Round (January-June 2014) shows that only 28 per cent and 21 per cent of patients in rural and urban areas respectively use the outpatient care provided by health facilities in the public sector. The corresponding figures for the usage of in-patient care are 42 per cent and 32 per cent. The mixed health system, therefore, remains largely dominated by the private sector, which provides services at widely varying costs and quality levels.
Public funding of health has been consistently low in India (approximately 1.3 per cent of GDP). As a result, out-of-pocket expenditure (OOPE) is 62 per cent of the total expenditure on health. In 2007, the central government launched the Rashtriya Swasthya Bima Yojana (RSBY) to cover hospital expenses of up to INR 30,000 for a family of five members living below the poverty line. Evaluation studies for RSBY have shown that while it did increase access to health care as well as non- medical health spending for the poor, it did not provide significant financial protection, perhaps due to the exclusion of spending on outpatient care, drugs and diagnostics. The decision to launch PM-JAY under Ayushman Bharat is a path breaking step towards Universal Health Coverage. It aims to cover 10.74 crore families at the bottom two quintiles with INR 5 lakh cover each year for secondary and tertiary care hospitalization. The PM-JAY will be implemented in alliance with state government schemes.
As per the NSSO 71st Round, out of the total OOPE, 63.5 per cent is on outpatient care. Of this, the largest expenditure (71 per cent) is on medicines. It is paradoxical that although India is one of the largest suppliers of generic drugs to the world, a significant proportion of the country’s population lacks access to essential medicines.
During the last four years, however, the government has taken significant steps to enhance access to medicines especially for the poor and middle classes. The prices 958 drugs have been capped along with the prices of cardiac stents and knee implants. The Pradhan Mantri Bhartiya Janaushadhi Pariyojana has been expanded from 99 functional stores in May, 2014 to 4,024 functional stores in September, 2018.
Constraints
There has been inadequate focus on comprehensive preventive care and primary care in the past.
The multiplicity of government-sponsored insurance schemes has resulted in the fragmentation of the risk pool. A sizeable risk pool comprising low- and high-risk individuals is imperative to ensure the viability and sustainability of insurance.
Since outpatient care, drugs and diagnostics are not covered under several government insurance schemes, people often delay seeking care until they are severely ill.
The coverage ceiling of RSBY is inadequate.
There is an acute shortage of motivated human resources for health, attributable at least partly to the poor incentives for government providers.
Access to drugs and medical devices at affordable prices is an essential ingredient of Universal Health Coverage. According to estimates by the Central Drugs and Standards Control Organization, around 84 per cent of the active pharmaceutical ingredients (APIs) for drugs manufactured in India are imported. This dependence on import of APIs has gone up more than fourfold between 2004 and 2013.
While the notification of medical devices rules is an important step, a clearly defined and comprehensive regulatory framework is required. Additionally, approximately 75 per cent of the current demand for devices is met through imports.
The prices of diagnostic tests can vary widely across the country. For example, a lipid profile test can cost Rs. 90 in some cities, going up to Rs. 7,110 in others.
Figure 30.1: Pillars of universal health coverage
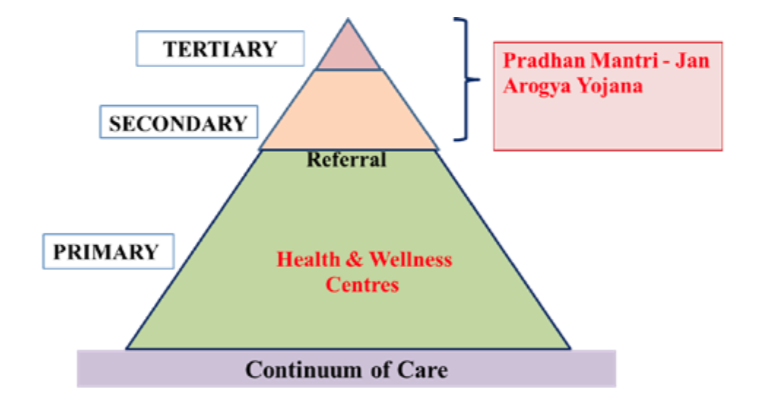 Note: Image taken from Niti Aayog - Strategy for New India@75 Document
Note: Image taken from Niti Aayog - Strategy for New India@75 Document
Way Forward
Recommendations pertaining to comprehensive primary healthcare, public health action and human resources for health are covered in other chapters of this document. Other strategies for overcoming the constraints listed are described below.
1. Roll out PM-JAYt
Digitize National Digital Health Authority
Establish the Ayushman Bharat-National Health Agency at the central level and counterpart institutions at the state and district levels for management of the PM-JAY.
Develop a robust, modular, scalable and interoperable IT platform as per standards formulated by the National Digital Health Authority to enable paperless and cashless transactions under the scheme.
Put in place mechanisms for fraud prevention, detection and control as well as for grievance redressal.
Design a comprehensive media and outreach strategy to increase awareness of the scheme among intended beneficiaries and other stakeholders.
Institutionalise health technology assessment at the central and state levels to determine the service packages to be covered under PM-JAY in the future.
Develop costing frameworks for determining accurate package rates for procedures.
Develop standard treatment guidelines for priority conditions.
Monitoring, evaluation and research
Put in place data analytics systems to guide strategic purchasing2 of health services, forecasting and generating policy inputs.
Institutionalize a mechanism for undertaking independent audits of the scheme.
Conduct research on the population-level impact of the programme including financial protection, healthcare access and health outcomes.
2. Galvanize health facilities in the public sector and engage the private sector
Provide Greater Autonomy to Public Hospitals
Provide greater autonomy to public hospitals to use claims money generated under PM-JAY to improve facilities, purchase the necessary drugs/tests and provide performance-based incentives to staff.
Strengthen district hospitals to conform to the Indian Public Health Standards.
Institutionalize ranking of district hospitals based on their performance on health indicators to foster competition and nudge them towards quality improvement.
Introduce appropriate gate-keeping mechanisms for adoption by the proposed health and wellness centres.
Reform the compensation system for professionals in public sector health facilities by shifting to a blended capitation mode of payment (part salary and part incentive based on achieving pre-agreed outcomes).
Trigger private investments in rural/supply deficit areas by providing appropriate incentives for empanelling hospitals.
E3. Ensure access to affordable drugs and medical devices
Institute a new Drug Price Control Order (DPCO)
Institute a new Drug Price Control Order (DPCO), which ensures rational drug prices by reducing trade margins.
Include consumables, in addition to drugs, in the DPCO to control undue profiteering.
Finalize the national pharmaceutical policy to enable access to affordable medicines, promote the use of generic drugs, clamp down on unfair marketing practices and give a boost to local manufacturing to reduce dependence on imports.
Formulate and implement the e-pharmacy policy to facilitate online access to quality medicines in a cost-effective and timely manner.
Review and iron out the challenges with the business model of Jan Aushadhi stores to ensure that they can function as self-sustaining entities and scale up rapidly across the country.
Find the best pathways for scaling up and adapting the process of bulk procurement of drugs adopted in states like Tamil Nadu and Rajasthan.
Boost domestic production of APIs by setting up six large API intermediate clusters as per the recommendations of the Katoch Committee.
Streamline regulatory processes including providing a single window clearance mechanism to manufacturers.
Introduce a separate Act for medical devices as per global best practises, so that medical devices are regulated separately from pharmaceuticals.
Formulate an appropriate pricing policy for medical devices and re-examine it periodically to ensure access to affordable devices for the population while also ensuring a sufficient return on investment.
Develop the National List of Essential Medical Devices along the lines of the National List of Essential Medicines to improve patient care, increase the affordability of tests, improve the regulation and quality of diagnostic tests, and promote the rational use of diagnostics.
4. Strengthen health research capacity
Research Consortia for Diseases of High Priority
Set up research consortia for diseases of high priority including neglected tropical diseases and emerging infections along the lines of the India TB Research and Development Corporation.
Identify at least 20 academic or research institutions at the regional level to act as hubs capable of training a minimum of 500 doctors every year.
Ensure the presence of at least one model rural health research unit in every state.
Cover the entire country with a network of viral research and diagnostic laboratories with a testing capacity of more than 15 lakh samples per year.
Identify key research areas in traditional medicine and facilitate collaborative research with modern systems of medicine.